来源:辛卡迪亚

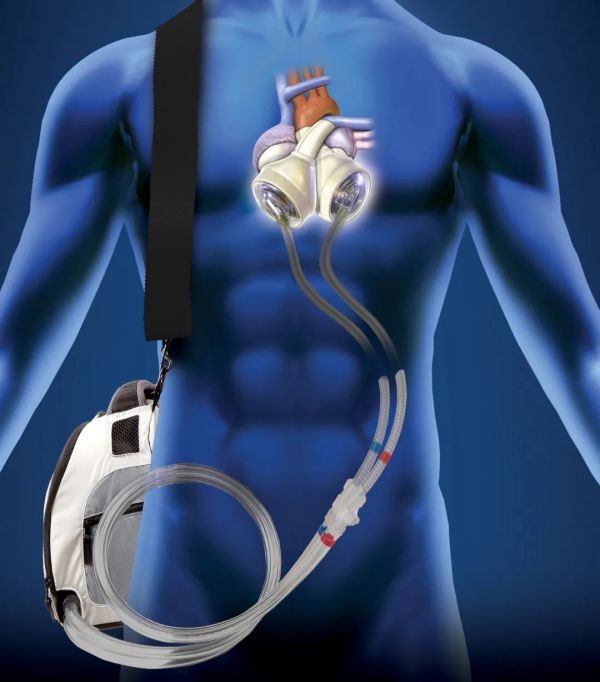
Over the course of his career, Emile Bacha, MD, Chief of the Division of Cardiac, Thoracic&Vascular Surgery at New York-Presbyterian/Columbia, has performed thousands of heart surgeries on children and infants. In December 2022, he performed what was a first in his career – and a first in the northeast– a total artificial heart (TAH) implant on one of the youngest pediatric patients.“There are about three or four places in the world that could have done a total artificial heart in a child like we did at Columbia,” says Dr. Bacha.This milestone was achievable at New York-Presbyterian/Columbia because of its long history treating heart failure in children. Experts in the Program for Pediatric Cardiomyopathy, Heart Failure, and Transplantation have been at the forefront of the development of new and innovative therapies, including the world’s first successful pediatric heart transplant in 1984.“New York-Presbyterian has always had a focus on pediatric heart and on innovation in pediatric heart really in trying to go as far as conceivably possible to bring benefit to children who quite frankly may not be able to survive otherwise,” says Jordan Orange, MD, PhD, Chair of Pediatrics at New York-Presbyterian/Columbia and Pediatrician-in-Chief at New York-Presbyterian Morgan Stanley Children’s Hospital.The comprehensive approach to treating pediatric heart disease at New York-Presbyterian/Columbia brings together a multidisciplinary team to care for each patient. Pediatric cardiologists, heart surgeons, nurse practitioners, geneticists, psychologists, neurologists, pharmacists, nutritionists, social workers, child life specialists, and physical and occupational therapists collaborate and play key roles in patients’ treatment and successful recovery unlike anywhere else.The Path to a Total Artificial Heart ImplantOne percent of all newborn babies are born with a congenital heart defect, and many of those progress to needing a heart transplant. Ventricular assist devices (VAD) were the original devices developed to provide mechanical assistance for heart function until a patient’s own heart recovers or is replaced by a heart transplant. “[With most assist devices,] it’s like adding an extra pump to the pump you already have,” says Dr. Bacha. “So, it’s like you have your own heart and you have a derivation of blood into an external pump.”While VADs are beneficial for many patients, the demand for heart transplants is greater than the donor organ availability which means that wait times to receive a transplant can be lengthy, as long as months or years. “It’s tough because sometimes [patients] don’t survive that time period because they’re typically in an ICU and sick,” says Dr. Bacha.The origin of the TAH – the next evolution of assist devices – dates back nearly 90 years, when doctors first experimented with implanting an artificial heart intervention into dogs.Over several decades, experiments and engineering took place until the first human patient was successfully implanted with a total artificial heart in 1982. "The TAH is very different from other assist devices,” says Dr. Bacha. “A total artificial heart is when you take out somebody’s heart and entirely and replace it with an artificial heart inside the patient’s chest.” This device is a pneumatically driven pulsatile system used for the temporary replacement of the heart’s ventricles and four valves. It serves as a bridge to transplantation for the sickest heart patients.The 50cc and 70cc total artificial heart implant (photo courtesy of SynCardia)Dr. Bacha and his team prepared for a year for the TAH, going through the surgical protocols, and working with SynCardia, the company that produces the TAH. Dr. Bacha also consulted with Yoshifumi Naka, MD, PhD, Surgical Director of Heart Failure, Heart Transplantation, and Mechanical Circulatory Support Programs at NewYork-Presbyterian/Weill Cornell Medicine, who had performed a TAH implantation in 2011 on a slightly older patient. “Dr. Naka is an extremely experienced surgeon and I remember him telling me about his patient who bled after surgery a lot,” says Dr. Bacha. “Typically, when you have bleeding from behind the heart, after a heart transplant, you can lift the transplanted heart and you can put a suture and fix the bleeding. You can go back on the heart-lung machine, lift the heart. You can do a lot of things. But here, it's a big metal [device] that you're putting in. It's not something you can lift and look behind. And the anastomosis are done to both atria in a posterior mediastinum behind that metal pump, so you can't move it. After it's implanted and it’s started and pumping blood, you can't lift it. The key move is to do everything you can from the get-go to avoid bleeding at any cost, and that was a direct connection with what Dr. Naka had told me about his case.”In late 2022, the right patient at New York-Presbyterian/Columbia was identified for the TAH implant. “Our patient had a heart transplant seven years ago and has suffered from very, very bad chronic rejection episodes to the degree that she was almost dying either from the rejection or from the high levels of medication needed to combat the rejection,” he says. “Therefore, the ideal solution was to…remove her heart and replace it with a total artificial heart."“Our patient had a heart transplant seven years ago and has suffered from very, very bad chronic rejection episodes to the degree that she was almost dying either from the rejection or from the high levels of medication needed to combat the rejection. Therefore, the ideal solution was to…remove her heart and replace it with a total artificial heart.”Implanting the TAH would allow the patient time to heal before receiving a new heart. “TAH lets us stop all immunosuppression, which is very exciting for us because it allows the immune system to be quiet,” says Sabrina Pia Law, MD, Director of the Pediatric VAD Program at NewYork-Presbyterian/Columbia. “This device would give her the opportunity to completely rehabilitate. She was really a perfect candidate for the device.”The Road to Recovery and a New HeartAs with any significant transplant procedure, the key to a successful recovery is having a dedicated, comprehensive care team. Following the surgery NewYork-Presbyterian/Columbia’s rehabilitation medicine team assisted with the daily routine in aiding the patient’s recovery. Joel Stein, MD, Chair of the Department of Rehabilitation and Regenerative Medicine at NewYork-Presbyterian/Columbia says that rehab plays a critical role in the treatment and recovery of heart failure patients. “Cardiac rehabilitation has been found effective in mitigating the symptoms of heart failure for patients managed medically and helping them regain greater function,” he says. “It can also help prepare patients for upcoming transplant or other surgical interventions by improving the patient’s ability to withstand and recover from surgery. For individuals after surgery, it plays a key role in regaining strength, endurance, and overall functional independence.”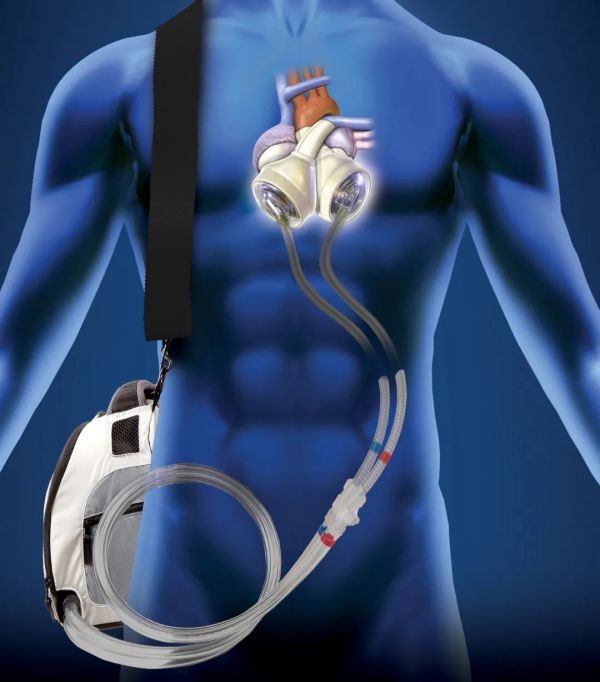 Total artificial heart in a human body (photo courtesy of SynCardia)Atara Sheinson, OTR/L, an occupational therapist, and Kathleen Riley, DPT, a physical therapist, worked closely with the VAD and heart failure teams, attending their meetings, to ensure that her recovery progressed and that all pertinent staff weighed in on her treatment. “We appreciate being involved so that rehab has a voice at the table and that we have the full support of this team during this phase of treatment,” says Sheinson. “She has this life-saving device, but if she doesn’t get stronger and is unable to do the things that are important to her, this would significantly impact her quality of life. She wouldn’t be up and moving without this team approach.”“She has this life-saving device, but if she doesn’t get stronger and is unable to do the things that are important to her, this would significantly impact her quality of life. She wouldn’t be up and moving without this team approach.”The cross-collaboration to bring patients back to optimal health is a hallmark of New York-Presbyterian. “You cannot do this without the entire team,” says Dr. Bacha. “The colleagues that you have here, the dedication that they show and how smart they are and how hardworking they are, is unbelievable. Without my colleagues, I might as well go do something else.”“The colleagues that you have here, the dedication that they show and how smart they are and how hardworking they are, is unbelievable. Without my colleagues, I might as well go do something else.”Sheinson and Riley worked with the patient for at least an hour every day that she has been medically stable following the implantation. They set treatment goals collaboratively with the patient to try and normalize and optimize things that she would normally do. But they also focused on getting her up walking so she could get listed for a new heart and worked on strength optimization, building up endurance, core, and proximal hip strength so that after her transplantation, she would have some preserved strength built up.At the end of March, the patient was listed for a new heart transplant. In mid-April, she underwent surgery to have the total artificial heart removed and the new heart implanted. The patient’s multidisciplinary care team will continue to collaborate on her recovery, including regular rehabilitation and cardiac monitoring, to put her on the path to the most successful outcome.
Total artificial heart in a human body (photo courtesy of SynCardia)Atara Sheinson, OTR/L, an occupational therapist, and Kathleen Riley, DPT, a physical therapist, worked closely with the VAD and heart failure teams, attending their meetings, to ensure that her recovery progressed and that all pertinent staff weighed in on her treatment. “We appreciate being involved so that rehab has a voice at the table and that we have the full support of this team during this phase of treatment,” says Sheinson. “She has this life-saving device, but if she doesn’t get stronger and is unable to do the things that are important to her, this would significantly impact her quality of life. She wouldn’t be up and moving without this team approach.”“She has this life-saving device, but if she doesn’t get stronger and is unable to do the things that are important to her, this would significantly impact her quality of life. She wouldn’t be up and moving without this team approach.”The cross-collaboration to bring patients back to optimal health is a hallmark of New York-Presbyterian. “You cannot do this without the entire team,” says Dr. Bacha. “The colleagues that you have here, the dedication that they show and how smart they are and how hardworking they are, is unbelievable. Without my colleagues, I might as well go do something else.”“The colleagues that you have here, the dedication that they show and how smart they are and how hardworking they are, is unbelievable. Without my colleagues, I might as well go do something else.”Sheinson and Riley worked with the patient for at least an hour every day that she has been medically stable following the implantation. They set treatment goals collaboratively with the patient to try and normalize and optimize things that she would normally do. But they also focused on getting her up walking so she could get listed for a new heart and worked on strength optimization, building up endurance, core, and proximal hip strength so that after her transplantation, she would have some preserved strength built up.At the end of March, the patient was listed for a new heart transplant. In mid-April, she underwent surgery to have the total artificial heart removed and the new heart implanted. The patient’s multidisciplinary care team will continue to collaborate on her recovery, including regular rehabilitation and cardiac monitoring, to put her on the path to the most successful outcome.